A Challenging Case of Leptospirosis
Main Article Content
Abstract
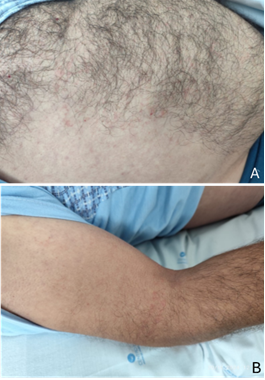
Leptospirosis is a significant zoonosis caused by the pathogenic bacterium Leptospira, which is transmitted directly or indirectly from animals to humans. It is a potentially severe but treatable disease. Its symptoms may mimic those of other infections, such as rickettsiosis, influenza, meningitis, or hepatitis. The disease spectrum ranges from subclinical infection to severe multi-organ failure with high mortality. Diagnosis is usually made through serology. However, a key limitation of serological testing is that antibodies are absent during the acute phase. In the early days of illness, the only sensitive and specific test is polymerase chain reaction (PCR). In Portugal, leptospirosis has gained increasing importance and is a notifiable disease. The authors present the case of a farmer with fever, headache, and rash who progressed to pancytopenia and hepatic cholestasis. A positive real-time PCR in a blood sample, specific for Leptospira, confirmed the diagnosis in the acute phase of the disease before antibody titers became detectable. Leptospira serologies remained negative. After antibiotic therapy and supportive care, the patient showed favorable clinical progression. Early diagnosis prevented complications. The authors report a challenging case of leptospirosis and aim to raise awareness about the importance of early diagnosis and appropriate treatment. Occupational exposure is a significant risk factor. Public health alert systems are essential to reduce risk. The need for rapid diagnosis at admission has driven the development of various PCR assays, which carry economic implications. Their advantage lies in confirming the diagnosis during the acute phase of disease, before antibody detection, and they may support improved public health control measures. However, molecular tests are still unavailable in some areas.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Belem F, Grilo J, Coutinho J, Filipe R, Rocha E. Um caso desafiante de Leptospirose. Case Rep Soc Port Med Interna. 2023 Apr-Jun;1(2).
Loscalzo J, Kasper DL, Jameson JL, Fauci AS, Longo DL, Hauser SL, editors. Leptospirosis. In: Harrison’s Principles of Internal Medicine. 21st ed. New York: McGraw-Hill Professional; 2022. p. 5334-52.
Moura S, Rio C, Gomes S, Santos Silva A. Distribuição temporal e geográfica da leptospirose humana diagnosticada em indivíduos residentes no norte de Portugal, 2014-2019. Repositório Científico do Instituto Nacional de Saúde.
Russell CD, Jones ME, O'Shea DT, Simpson KJ, Mitchell A, Laurenson IF. Challenges in the diagnosis of leptospirosis outwith endemic settings: a Scottish single centre experience. J R Coll Physicians Edinb. 2018;48:9-15. doi: 10.4997/JRCPE.2018.102.
Mukadi P, Tabei K, Edwards T, Brett-Major DM, Smith C, Kitashoji E, et al. Antibiotics for treatment of leptospirosis. Cochrane Database Syst Rev. 2022 Nov;CD014959. doi: 10.1002/14651858.CD014959.
Oliveira S. Leptospirose – Guia de vigilância em saúde. 3ª ed. Brasília: Ministério da Saúde; 2019. (Vol. 9).
Musso D, La Scola B. Laboratory diagnosis of leptospirosis: a challenge. J Microbiol Immunol Infect. 2013;46:245-52.
Neto F, Diniz R, et al. Case report: The use of venovenous extracorporeal membrane oxygenation in the treatment of acute respiratory distress syndrome in severe leptospirosis. Braz J Case Rep. 2025;5(1):bjcr40.
Gancheva G. Leptospirosis in elderly patients. Braz J Infect Dis. 2013;17(5):592-5.
Daher E, Lima R, et al. Clinical presentation of leptospirosis: a retrospective study of 201 patients in a metropolitan city of Brazil. Braz J Infect Dis. 2010;14(1):3-10.
Petakh P, Behzadi P, Oksenych V, Kamyshnyi O. Current treatment options for leptospirosis: a mini-review. Front Microbiol. 2024 Apr 25;15:1403765. doi: 10.3389/fmicb.2024.1403765.
UpToDate. Leptospirosis: epidemiology, microbiology, clinical manifestations, and diagnosis. Available from: https://www.uptodate.com/contents/leptospirosis-epidemiology-microbiology-clinical-manifestations-and-diagnosis
Gomes A, Gazola D, et al. Leptospirosis: an update – part 1 of 2: etiology, ecology, epidemiology, prophylaxis and control. Braz J Health Rev. 2022 May-Jun;5(3):11361-72.
Pinto V, Senthilkumar K, et al. Current methods for the diagnosis of leptospirosis: issues and challenges. J Microbiol Methods. 2022 Apr;195:106438.
Woods K, Nic-Fhogartaigh C. A comparison of two molecular methods for diagnosing leptospirosis from three different sample types in patients presenting with fever in Laos. Clin Microbiol Infect. 2018 Sep;24(9):1017.e1-1017.e7.
Esteves L, Bulhões S, et al. Diagnosis of human leptospirosis in a clinical setting: real-time PCR high resolution melting analysis for detection of Leptospira at the onset of disease. Sci Rep. 2018;8:9213.
Waggoner JJ, Pinsky BA. Molecular diagnostics for human leptospiroses. Curr Opin Infect Dis. 2016 Oct;29(5):440-5.
Balassiano I, Pereira M. Diagnostic microbiology and infectious disease. Diagn Microbiol Infect Dis. 2012;74:11-5.
Musso D, La Scola B. Laboratory diagnosis of leptospiroses: a challenge. J Microbiol Immunol Infect. 2013;46:245-52.
Mandell GL, Bennett JE, Dolin R. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 9th ed. Phi-ladelphia: Elsevier; 2019. p. 2898-2904.
Verma V, Goyal M, et al. Recent advances in the diagnosis of leptospiroses. Front Biosci (Landmark Ed). 2020 Mar;25:1655-81.
Hillmann W, Chung M, et al. A 37-year-old man with fever, myalgia, jaundice and respiratory failure. Case records of the Massachusetts General Hospital. N Engl J Med. 2024 Oct.