The Role of the Autopsy During the COVID-19 Pandemic in a Case of Sudden Death with Fatal Hemorrhage and Thrombosis Post chAdox1nCoV-19 VACCINE - A Case Review
Main Article Content
Abstract
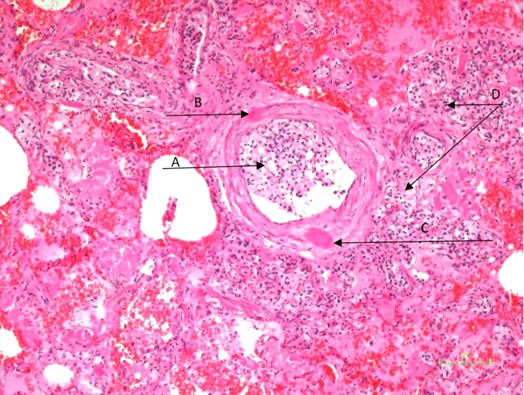
This case report describes an elderly patient who experienced sudden death from fulminant pulmonary, gastrointestinal and nasal hemorrhage one day after receiving his second dose of the AstraZeneca ChAdox1nCoV-19 vaccine, during the SARS-CoV-2 pandemic. The patient was PCR negative for SARS-CoV-2, but had thrombocytopenia, erythroblastosis and markedly elevated D-Dimer levels. The clinical diagnoses considered included hypovolemic shock, Vaccine-Induced Immune Thrombotic Thrombocytopenia (VITT), PCR negative SARS-CoV-2 infection, Vaccine-Associated Enhanced Disease (VAED), Vaccine-induced Covid-19 mimicry Syndrome and Adenovirus induced thrombocytopenia and thrombosis. The autopsy findings revealed diffuse pulmonary hemorrhage, thrombosis of the microvascular system of the lungs, myocardium and kidneys, together with metastatic foamy cell prostate carcinoma to the lung and bone marrow. Disseminated Intravascular coagulation (DIC) secondary to advanced prostate cancer remained a significant differential diagnosis. This case report highlights the complexity of diagnosing (VITT) and the importance of considering other potential causes of thrombocytopenia and thrombosis, including the presence of solid tumors, particularly in elderly patients. The autopsy provided crucial insights into the patient’s condition.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Platto S, Wang Y, Zhou J, Carafoli E. History of the COVID-19 pandemic: Origin, explosion, worldwide spreading. Biochem Biophys Res Commun. 2021 Jan 29;538:14-23. doi: 10.1016/j.bbrc.2020.10.087.
COVID Live Update: https//www.worldmeters.info>coronavirus. Accessed June 1st 2025.
Williams SV, Vusirikala A, Ladhani SN, Fernandez Ruiz De Olano E, Iyanger N, Aiano F, Stoker K, Gopal Rao G, John L, Patel B, Andrews N, Dabrera G, Ramsay M, Brown KE, Lopez Bernal J, Saliba V. An outbreak caused by the SARS-CoV-2 Delta (B.1.617.2) variant in a care home after partial vaccination with a single dose of the COVID-19 vaccine Vaxzevria, London, England, April 2021. Euro Surveill. 2021 Jul;26(27). doi: 10.2807/1560-7917.ES.2021.26.27.2100626.
Wibawa T. COVID-19 vaccine research and development: ethical issues. Trop Med Int Health. 2021 Jan;26(1):14-19. doi: 10.1111/tmi.13503.
Colella, G., Orlandi, M. & Cirillo, N. Bell’s palsy following COVID-19 vaccination. J Neurol 268, 3589–3591 (2021). https://doi.org/10.1007/s00415-021-10462-4
Menni C, Klaser K, May A, Polidori L, Capdevila J, Louca P, Sudre CH, Nguyen LH, Drew DA, Merino J, Hu C, Selvachandran S, Antonelli M, Murray B, Canas LS, Molteni E, Graham MS, Modat M, Joshi AD, Mangino M, Hammers A, Goodman AL, Chan AT, Wolf J, Steves CJ, Valdes AM, Ourselin S, Spector TD.. Vaccine side-effects and SARS-CoV-2 infection after vaccination in users of the COVID Symptom Study app in the UK: a prospective observational study. Lancet Infect Dis. 2021 Jul;21(7):939-949. doi: 10.1016/S1473-3099(21)00224-3.
Gargano JW, Wallace M, Hadler SC, Langley G, Su JR, Oster ME, Broder KR, Gee J, Weintraub E, Shimabukuro T, Scobie HM, Moulia D, Markowitz LE, Wharton M, McNally VV, Romero JR, Talbot HK, Lee GM, Daley MF, Oliver SE. Use of mRNA COVID-19 Vaccine After Reports of Myocarditis Among Vaccine Recipients: Update from the Advisory Committee on Im-munization Practices - United States, June 2021. MMWR Morb Mortal Wkly Rep. 2021 Jul 9;70(27):977-982. doi: 10.15585/mmwr.mm7027e2.
Lai CC, Ko WC, Chen CJ, Chen PY, Huang YC, Lee PI, Hsueh PR. COVID-19 vaccines and thrombosis with thrombocytopenia syndrome. Expert Rev Vaccines. 2021 Aug;20(8):1027-1035. doi: 10.1080/14760584.2021.1949294.
Finsterer J. Exacerbating Guillain-Barré Syndrome Eight Days after Vector-Based COVID-19 Vaccination. Case Rep Infect Dis. 2021 May 8;2021:3619131. doi: 10.1155/2021/3619131.
CDC COVID-19 Vaccine Breakthrough Case Investigations Team. COVID-19 Vaccine Breakthrough Infections Reported to CDC - United States, January 1-April 30, 2021. MMWR Morb Mortal Wkly Rep. 2021 May 28;70(21):792-793. doi: 10.15585/mmwr.mm7021e3.
Tiboni M, Casettari L, Illum L. Nasal vaccination against SARS-CoV-2: Synergistic or alternative to intramuscular vaccines? Int J Pharm. 2021 Jun 15;603:120686. doi: 10.1016/j.ijpharm.2021.120686.
Bleier BS, Ramanathan M Jr, Lane AP. COVID-19 Vaccines May Not Prevent Nasal SARS-CoV-2 Infection and Asymptomatic Transmission. Otolaryngol Head Neck Surg. 2021 Feb;164(2):305-307. doi: 10.1177/0194599820982633.
Adult Autopsy standards. mdhero.com. Accessed June 1 2025.
Cenariu D, Iluta S, Zimta AA, Petrushev B, Qian L, Dirzu N, Tomuleasa C, Bumbea H, Zaharie F. Extramedullary Hemato-poiesis of the Liver and Spleen. J Clin Med. 2021 Dec 13;10(24):5831. doi: 10.3390/jcm10245831. PMID: 34945127; PMCID: PMC8707658.
Romero-Laorden N, Jara C, Pinedo F, de la Cruz R, Hernando S, et al. (2015) Macroscopic Extramedullary Hematopoiesis Resembling .Hepatic Metastases in Prostate Cancer. J Cytol Histol 6: 356. doi:10.4172/2157-7099.1000356)
Yang H, He F, Yuan T, Xu W, Cao Z. Clinical features and treatment of bone marrow metastasis. Oncol Lett. 2023 Jun 16;26(2):332. doi: 10.3892/ol.2023.13918. PMID: 37415634; PMCID: PMC10320432.
Barisas, D.A.G., Choi, K. Extramedullary hematopoiesis in cancer. Exp Mol Med 56, 549–558 (2024). https://doi.org/10.1038/s12276-024-01192-4.
Rawla P. Epidemiology of Prostate Cancer. World J Oncol. 2019 Apr;10(2):63-89. doi: 10.14740/wjon1191.
Bunker CH, Patrick AL, Konety BR, Dhir R, Brufsky AM, Vivas CA, Becich MJ, Trump DL, Kuller LH. High prevalence of screening-detected prostate cancer among Afro-Caribbeans: the Tobago Prostate Cancer Survey. Cancer Epidemiol Bi-omarkers Prev. 2002 Aug;11(8):726-9. PMID: 12163325.
George D. Paul L. Daisley H. Cancer burden in Tobago W.I . WIMJ Supplement Vol 71; April 25-27,2024. O-28, p35 ISSN 2309-5830.)
Griffin PT, Jaglal M. Metastatic prostate cancer mimicking thrombotic thrombocytopenic purpura. Blood. 2015 Feb 19;125(8):1349. doi: 10.1182/blood-2014-11-608828.
Betsch DM, Gray S, Zed SE. A case of metastatic prostate cancer and immune thrombocytopenia. Curr Oncol. 2017 Oct;24(5):e434-e436. doi: 10.3747/co.24.3592.
Liu X, Liang X, Liang J, Li Y, Wang J. Immune Thrombocytopenia Induced by Immune Checkpoint Inhibitors in Solid Cancer: Case Report and Literature Review. Front Oncol. 2020 Dec 7;10:530478. doi:10.3389/fonc.2020.530478.
Arepally GM, Ortel TL. Vaccine-induced immune thrombotic thrombocytopenia: what we know and do not know. Blood. 2021 Jul 29;138(4):293-298. doi: 10.1182/blood.2021012152. Epub 2021 Jun 1. Erratum in: Blood. 2023 Feb 16;141(7):808. doi: 10.1182/blood.2022017479.
Ziani I, Ibrahimi A, Bellouki O, Zaoui Y, Housseini YL, Zouidia F, Sayegh HE, Benslimane L, Nouini Y. Medullary Aplasia Revealing a Metastatic Prostatic Adenocarcinoma. Case Rep Urol. 2021 Feb 23;2021:8898130. doi: 10.1155/2021/8898130.
Smock KJ, Perkins SL. Thrombocytopenia: an update. Int J Lab Hematol. 2014 Jun;36(3):269-78. doi: 10.1111/ijlh.12214.
McAnearney S, Drain M. A case of pulmonary tumour thrombotic microangiopathy. Respir Med Case Rep. 2015 Apr 30;16:7-10. doi: 10.1016/j.rmcr.2015.04.006.
Weitz IC. Thrombotic Microangiopathy in Cancer. Semin Thromb Hemost. 2019 Jun;45(4):348-353. doi: 10.1055/s-0039-1687893.
Story M, Kwon SK, Robinson R, Fortis S. Acute cor pulmonale due to pulmonary tumour thrombotic microangiopathy from renal cell carcinoma. BMJ Case Rep 2017;2017:bcr-2017–bcr- 219730)
Kamada H, Ota H, Terui Y, Sugimura K, Fukui S, Shimokawa H, Takase K. Three cases of pulmonary tumour thrombotic microangiopathy (PTTM): Challenge in antemortem diagnosis using lung perfusion blood volume images by dual-energy computed tomography. Eur J Radiol Open. 2020 Jan 28;7:100212. doi: 10.1016/j.ejro.2020.01.001.
Schwartzman W, Wilson P, Gray Z, Wang J. Management of Prostate Cancer Associated Disseminated Intravascular Coagu-lation (DIC): A Multidisciplinary and Individualized Approach [Internet]. Cardiology and Cardiovascular Medicine. IntechOpen; 2024. Available from: http://dx.doi.org/10.5772/intechopen.1008297 ]
Shirbhate E, Pandey J, Patel VK, Kamal M, Jawaid T, Gorain B, Kesharwani P, Rajak H. Understanding the role of ACE-2 re-ceptor in pathogenesis of COVID-19 disease: a potential approach for therapeutic intervention. Pharmacol Rep. 2021 Dec;73(6):1539-1550. doi: 10.1007/s43440-021-00303-6.
Daisley H Jr, Rampersad A, Daisley M, Ramdin A, Acco O, Narinesingh F, Humphrey O. COVID-19: a closer look at the pathology in two autopsied cases. Is the pericyte at the center of the pathological process in COVID-19? Autops Case Rep. 2021 May 6;11:e2021262. doi: 10.4322/acr.2021.262.
Daisley H, Acco O, Joseph H, Daisley J, Daisley M. (2024). The Cardiac pathophysiology of Covid-19. Brazilian Journal of Case Reports, 5(1), bjcr43. https://doi.org/10.52600/2763-583X.bjcr.2025.5.1.bjcr43 )
Almehdi AM, Khoder G, Alchakee AS, Alsayyid AT, Sarg NH, Soliman SSM. SARS-CoV-2 spike protein: pathogenesis, vac-cines, and potential therapies. Infection. 2021 Oct;49(5):855-876. doi: 10.1007/s15010-021-01677-8.
The DELVE Initiative (2020), SARS-CoV-2 Vaccine Development & Implementation; Scenarios, Options, Key Decisions. DELVE Report No. 6. Published 01 October 2020. Available from https://rsdelve.github.io/reports/2020/10/01/covid19-vaccination-report.html . Accessed June 1 2025
Yasunori Watanabe, Luiza Mendonça, Elizabeth R. Allen, Andrew Howe, Mercede Lee, Joel D. Allen, Himanshi Chawla, David Pulido, Francesca Donnellan, Hannah Davies, Marta Ulaszewska, Sandra Belij-Rammerstorfer, Susan Morris, Anna-Sophia Krebs, Wanwisa Dejnirattisai, Juthathip Mongkolsapaya, Piyada Supasa, Gavin R. Screaton, Catherine M. Green, Teresa Lambe, Peijun Zhang, Sarah C. Gilbert, and Max Crispin Native-like SARS-CoV-2 Spike Glycoprotein Expressed by ChAdOx1 nCoV-19/AZD1222 Vaccine. ACS Cent Sci. 2021 Apr 28;7(4):594-602. doi: 10.1021/acscentsci.1c00080.
Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, Angus B, Baillie VL, Barnabas SL, Bhorat QE, Bibi S, Briner C, Cicconi P, Collins AM, Colin-Jones R, Cutland CL, Darton TC, Dheda K, Duncan CJA, Emary KRW, Ewer KJ, Fairlie L, Faust SN, Feng S, Ferreira DM, Finn A, Goodman AL, Green CM, Green CA, Heath PT, Hill C, Hill H, Hirsch I, Hodgson SHC, Izu A, Jackson S, Jenkin D, Joe CCD, Kerridge S, Koen A, Kwatra G, Lazarus R, Lawrie AM, Lelliott A, Libri V, Lillie PJ, Mallory R, Mendes AVA, Milan EP, Minassian AM, McGregor A, Morrison H, Mujadidi YF, Nana A, O'Reilly PJ, Padayachee SD, Pittella A, Plested E, Pollock KM, Ramasamy MN, Rhead S, Schwarzbold AV, Singh N, Smith A, Song R, Snape MD, Sprinz E, Sutherland RK, Tarrant R, Thomson EC, Török ME, Toshner M, Turner DPJ, Vekemans J, Villafana TL, Watson MEE, Williams CJ, Douglas AD, Hill AVS, Lambe T, Gilbert SC, Pollard AJ; Oxford COVID Vaccine Trial Group. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021 Jan 9;397(10269):99-111. doi: 10.1016/S0140-6736(20)32661-1.
Lee EJ, Cines DB, Gernsheimer T, Kessler C, Michel M, Tarantino MD, Semple JW, Arnold DM, Godeau B, Lambert MP, Bussel JB. Thrombocytopenia following Pfizer and Moderna SARS-CoV-2 vaccination. Am J Hematol. 2021 May 1;96(5):534-537. doi: 10.1002/ajh.26132. Epub 2021 Mar 9. PMID: 33606296; PMCID: PMC8014568.
Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S. Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination. N Engl J Med. 2021 Jun 3;384(22):2092-2101. doi: 10.1056/NEJMoa2104840.
Cines DB, Bussel JB. SARS-CoV-2 Vaccine-Induced Immune Thrombotic Thrombocytopenia. N Engl J Med. 2021 Jun 10; 384(23):2254-2256. doi: 10.1056/NEJMe2106315.
Dotan A, Shoenfeld Y. Perspectives on vaccine induced thrombotic thrombocytopenia. J Autoimmun. 2021 Jul;121:102663. doi: 10.1016/j.jaut.2021.102663.
Arepally GM, Padmanabhan A. Heparin-Induced Thrombocytopenia: A Focus on Thrombosis. Arterioscler Thromb Vasc Biol. 2021 Jan;41(1):141-152. doi: 10.1161/ATVBAHA.120.315445.
Pomara C, Sessa F, Ciaccio M, Dieli F, Esposito M, Garozzo SF, Giarratano A, Prati D, Rappa F, Salerno M, Tripodo C, Zamboni P, Mannucci PM. Post-mortem findings in vaccine-induced thrombotic thombocytopenia. Haematologica. 2021 Aug 1;106(8):2291-2293. doi: 10.3324/haematol.2021.279075. PMID: 34011138; PMCID: PMC8327725.
Kowarz E, Krutzke L, Külp M, Streb P, Larghero P, Reis J, Bracharz S, Engler T, Kochanek S, Marschalek R. Vaccine-induced COVID-19 mimicry syndrome. Elife. 2022 Jan 27;11:e74974. doi: 10.7554/eLife.74974. PMID: 35084333; PMCID: PMC8846585.
Geeraerts T, Guilbeau-Frugier C, Garcia C, Memier V, Raposo N, Bonneville F, Gales C, Darcourt J, Voisin S, Ribes A, Piel-Julian M, Bounes F, Albucher JF, Roux FE, Izopet J, Telmon N, Olivot JM, Sié P, Bauer J, Payrastre B, Liblau RS. Im-munohistologic Features of Cerebral Venous Thrombosis Due to Vaccine-Induced Immune Thrombotic Thrombocytopenia. Neurol Neuroimmunol Neuroinflamm. 2023 May 26;10(4):e200127. doi: 10.1212/NXI.0000000000200127. PMID: 37236806; PMCID: PMC10219108.
Angeli F, Reboldi G, Trapasso M, Zappa M, Spanevello A, Verdecchia P. COVID-19,vaccines and deficiency of ACE2 and other angiotensinases. Closing the loop on the "Spike effect". Eur J Intern Med. 2022 Sep;103:23-28. doi: 10.1016/j.ejim.2022.06.015.
Devaux CA, Camoin-Jau L. Molecular Mimicry of the Viral Spike in the SARS-CoV-2 Vaccine Possibly Triggers Transient Dysregulation of ACE2, Leading to Vascular and Coagulation Dysfunction Similar to SARS-CoV-2 Infection. Viruses. 2023 Apr 25;15(5):1045. doi: 10.3390/v15051045.
Zhang S, Liu Y, Wang X, Yang L, Li H, Wang Y, Liu M, Zhao X, Xie Y, Yang Y, Zhang S, Fan Z, Dong J, Yuan Z, Ding Z, Zhang Y, Hu L. SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19. J Hematol Oncol. 2020 Sep 4;13(1):120. doi: 10.1186/s13045-020-00954-7. PMID: 32887634; PMCID: PMC7471641.
Chamling B, Vehof V, Drakos S, Weil M, Stalling P, Vahlhaus C, Mueller P, Bietenbeck M, Reinecke H, Meier C, Yilmaz A. Occurrence of acute infarct-like myocarditis following COVID-19 vaccination: just an accidental co-incidence or rather vac-cination-associated autoimmune myocarditis? Clin Res Cardiol. 2021 Nov;110(11):1850-1854. doi: 10.1007/s00392-021-01916-w.
Nicin L, Abplanalp WT, Mellentin H, Kattih B, Tombor L, John D, Schmitto JD, Heineke J, Emrich F, Arsalan M, Holubec T, Walther T, Zeiher AM, Dimmeler S. Cell type-specific expression of the putative SARS-CoV-2 receptor ACE2 in human hearts. Eur Heart J. 2020 May 14;41(19):1804-1806. doi: 10.1093/eurheartj/ehaa311. PMID: 32293672; PMCID: PMC7184464.
Brogna C, Cristoni S, Marino G, Montano L, Viduto V, Fabrowski M, Lettieri G, Piscopo M. Detection of recombinant Spike protein in the blood of individuals vaccinated against SARS-CoV-2: Possible molecular mechanisms. Proteomics Clin Appl. 2023 Nov;17(6):e2300048. doi: 10.1002/prca.202300048. Epub 2023 Aug 31. PMID: 37650258.
Devaux C, Camoin-Jau L. Transient Blood Release of Synthetic SARS-Cov-2 Spike Protein after mRNA-Based COVID-19 Vaccination Possibly Contributes to ACE2 Dysfunction Leading to Rare Cases of Myocarditis. Cardiology and Cardiovascular Medicine. 8 (2024): 307-329 DOI: 10.26502/fccm.92920392.
Yaamika H, Muralidas D, Elumalai K. Review of adverse events associated with COVID-19 vaccines, highlighting their frequencies and reported cases. J Taibah Univ Med Sci. 2023 Sep 5;18(6):1646-1661. doi: 10.1016/j.jtumed.2023.08.004. )
Nicolson PLR, Abrams ST, Amirthalingam G, et al. Understanding mechanisms of thrombosis and thrombocytopenia with adenoviral SARS-CoV-2 vaccines: a comprehensive synopsis. Southampton (UK): National Institute for Health and Care Research; 2025 Jul. (Efficacy and Mechanism Evaluation, No. 12.07.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK616006/doi: 10.3310/FFSS9010.)
Shimony, N. “Analysis of Adenoviral Attachment to Human Platelets.” Virology Journal, 2009. doi:10.1186/1743-422X-6-25.
Othman M, Labelle A, Mazzetti I, Elbatarny HS, Lillicrap D. Adenovirus-induced thrombocytopenia: the role of von Wil-lebrand factor and P-selectin in mediating accelerated platelet clearance. Blood. 2007 Apr 1;109(7):2832-9. doi: 10.1182/blood-2006-06-032524.
Rand ML, Wright JF. Virus-associated idiopathic thrombocytopenic purpura. Transfus Sci. 1998 Sep;19(3):253-9. doi: 10.1016/s0955-3886(98)00039-3.
Othman M, Baker AT, Gupalo E, Elsebaie A, Bliss CM, Rondina MT, Lillicrap D, Parker AL. To clot or not to clot? Ad is the question-Insights on mechanisms related to vaccine-induced thrombotic thrombocytopenia. J Thromb Haemost. 2021 Nov;19(11):2845-2856. doi: 10.1111/jth.15485. Epub 2021 Aug 23. Erratum in: J Thromb Haemost. 2023 Apr;21(4):1066. doi: 10.1016/j.jtha.2023.01.022. PMID: 34351057; PMCID: PMC8420166.
Cichon G, Schmidt HH, Benhidjeb T, Löser P, Ziemer S, Haas R, Grewe N, Schnieders F, Heeren J, Manns MP, Schlag PM, Strauss M. Intravenous administration of recombinant adenoviruses causes thrombocytopenia, anemia and erythroblastosis in rabbits. J Gene Med. 1999 Sep-Oct;1(5):360-71. doi: 10.1002/(SICI)1521-2254(199909/10)1:5<360::AID-JGM54>3.0.CO;2-Q. PMID: 10738553.
Folegatti PM, Ewer KJ, Aley PK, Angus B, Becker S, Belij-Rammerstorfer S, Bellamy D, Bibi S, Bittaye M, Clutterbuck EA, Dold C, Faust SN, Finn A, Flaxman AL, Hallis B, Heath P, Jenkin D, Lazarus R, Makinson R, Minassian AM, Pollock KM, Ramasamy M, Robinson H, Snape M, Tarrant R, Voysey M, Green C, Douglas AD, Hill AVS, Lambe T, Gilbert SC, Pollard AJ; Oxford COVID Vaccine Trial Group. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a prelim-inary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020 Aug 15;396(10249):467-478. doi: 10.1016/S0140-6736(20)31604-4. Epub 2020 Jul 20. Erratum in: Lancet. 2020 Aug 15;396(10249):466. doi: 10.1016/S0140-6736(20)31687-1. Erratum in: Lancet. 2020 Dec 12;396(10266):1884. doi: 10.1016/S0140-6736(20)32597-6. PMID: 32702298; PMCID: PMC7445431.
Daisley H, Acco O, Daisley M, George D, Paul L, Rampersad A, Daisley J. COVID-19 shed light on Virchow's law of thrombosis. Autops Case Rep. 2024 Aug 28;14:e2024512. doi: 10.4322/acr.2024.512. PMID: 39372069; PMCID: PMC11452080.
Li Y, Yao L, Li J, Chen L, Song Y, Cai Z, Yang C. Stability issues of RT-PCR testing of SARS-CoV-2 for hospitalized patients clinically diagnosed with COVID-19. J Med Virol. 2020 Jul;92(7):903-908. doi: 10.1002/jmv.25786.
Li D, Wang D, Dong J, Wang N, Huang H, Xu H, Xia C. False-Negative Results of Real-Time Reverse-Transcriptase Polymerase Chain Reaction for Severe Acute Respiratory Syndrome Coronavirus 2: Role of Deep-Learning-Based CT Diagnosis and In-sights from Two Cases. Korean J Radiol. 2020). doi: 10.3348/kjr.2020.0146.
Siddiqui A, Singh S, Khan Z, Foster A, Atere M, Nfonoyim JM. What are we missing? Three cases of severe COVID-19 pneumonia with negative testing. SAGE Open Med Case Rep. 2020 Oct 15;8:2050313X20965410. doi: 10.1177/2050313X20965410.
Waked R, Makhoul J, Saliba G, Chehata N, Mortada S, Zoghbi A, Choucair J, Haddad E. Are two consecutive negative RT-PCR results enough to rule out COVID-19? New Microbes New Infect. 2020 Sep;37:100750. doi: 10.1016/j.nmni.2020.100750. Epub 2020 Aug 27. PMID: 32874594; PMCID: PMC7451052.
Malgaj Vrecko M, Veceric-Haler Z. Coronavirus Disease 2019-Associated Thrombotic Microangiopathy. J Hematol. 2022 Aug;11(4):148-153. doi: 10.14740/jh1019. Epub 2022 Aug 30..
Schneider J, Mijočević H, Ulm K, Ulm B, Weidlich S, Würstle S, Rothe K, Treiber M, Iakoubov R, Mayr U, Lahmer T, Rasch S, Herner A, Burian E, Lohöfer F, Braren R, Makowski MR, Schmid RM, Protzer U, Spinner C, Geisler F. SARS-CoV-2 serology increases diagnostic accuracy in CT-suspected, PCR-negative COVID-19 patients during pandemic. Respir Res. 2021 Apr 23;22(1):119. doi: 10.1186/s12931-021-01717-9. PMID: 33892720; PMCID: PMC8062836.
Hasanah M, Aulia FA, Wardhani P, Aryati. Comparison of SARS-CoV-2 virus detection using the Xpert Xpress rapid molecular test on Abbott M2000 Real-Time System: a cross-sectional study. Ann Med Surg (Lond). 2023 May 10;85(6):2559-2563. doi: 10.1097/MS9.0000000000000802.
Goldenberger D, Leuzinger K, Sogaard KK, Gosert R, Roloff T, Naegele K, Cuénod A, Mari A, Seth-Smith H, Rentsch K, Hinić V, Hirsch HH, Egli A. Brief validation of the novel GeneXpert Xpress SARS-CoV-2 PCR assay. J Virol Methods. 2020 Oct;284:113925. doi: 10.1016/j.jviromet.2020.113925. Epub 2020 Jul 10. PMID: 32659240; PMCID: PMC7351036.
Arnold S Monto, Epidemiology of viral respiratory infections, The American Journal of Medicine, Volume 112, Issue 6, Supplement 1,2002,Pages 4-12,ISSN 0002-9343.
Daisley H Jr, Rampersad A, Daisley M, Ramdin A, Acco O. Coronavirus 229E with Rhinovirus co-infection causing severe acute respiratory distress syndrome with thrombotic microangiopathy and death during Covid-19 pandemic: lessons to be learnt. Autops Case Rep. 2020 Aug 14;10(3):e2020194. doi: 10.4322/acr.2020.194
Trinidad and Tobago: WHO Coronavirus Disease ( COVID_19). https://covid19.who.int) Accessed June 1st 2025
Genomic sequencing of SARS-CoV-2: a guide to implementation for maximum impact on public health. Geneva: World Health Organization; 2021. Licence: CC BY-NC-SA 3.0 IGO.)
COVID-19 Delta variant detected in 98 countries, continues to evolve and mutate, warns WHO. Https//news.un.org
Voysey M, Costa Clemens SA, Madhi SA, Weckx LY, Folegatti PM, Aley PK, Angus B, Baillie VL, Barnabas SL, Bhorat QE, Bibi S, Briner C, Cicconi P, Clutterbuck EA, Collins AM, Cutland CL, Darton TC, Dheda K, Dold C, Duncan CJA, Emary KRW, Ewer KJ, Flaxman A, Fairlie L, Faust SN, Feng S, Ferreira DM, Finn A, Galiza E, Goodman AL, Green CM, Green CA, Greenland M, Hill C, Hill HC, Hirsch I, Izu A, Jenkin D, Joe CCD, Kerridge S, Koen A, Kwatra G, Lazarus R, Libri V, Lillie PJ, Marchevsky NG, Marshall RP, Mendes AVA, Milan EP, Minassian AM, McGregor A, Mujadidi YF, Nana A, Padayachee SD, Phillips DJ, Pittella A, Plested E, Pollock KM, Ramasamy MN, Ritchie AJ, Robinson H, Schwarzbold AV, Smith A, Song R, Snape MD, Sprinz E, Sutherland RK, Thomson EC, Török ME, Toshner M, Turner DPJ, Vekemans J, Villafana TL, White T, Williams CJ, Douglas AD, Hill AVS, Lambe T, Gilbert SC, Pollard AJ; Oxford COVID Vaccine Trial Group. Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: a pooled analysis of four randomised trials. Lancet. 2021 Mar 6;397(10277):881-891. doi: 10.1016/S0140-6736(21)00432-3. Epub 2021 Feb 19. Erratum in: Lancet. 2021 Mar 6;397(10277):880. doi: 10.1016/S0140-6736(21)00515-8. PMID: 33617777; PMCID: PMC7894131.
Planas D, Veyer D, Baidaliuk A, Staropoli I, Guivel-Benhassine F, Rajah MM, Planchais C, Porrot F, Robillard N, Puech J, Prot M, Gallais F, Gantner P, Velay A, Le Guen J, Kassis-Chikhani N, Edriss D, Belec L, Seve A, Courtellemont L, Péré H, Hocqueloux L, Fafi-Kremer S, Prazuck T, Mouquet H, Bruel T, Simon-Lorière E, Rey FA, Schwartz O. Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature. 2021 Aug;596(7871):276-280. doi: 10.1038/s41586-021-03777-9. Epub 2021 Jul 8. PMID: 34237773.
Gopinath S, Ishak A, Dhawan N, Poudel S, Shrestha PS, Singh P, Xie E, Tahir P, Marzaban S, Michel J, Michel G. Characteristics of COVID-19 Breakthrough Infections among Vaccinated Individuals and Associated Risk Factors: A Systematic Review. Trop Med Infect Dis. 2022.
Saade C, Bruel T, Vrignaud LL, Killian M, Drouillard A, Barateau V, Espi M, Mariano N, Mignon C, Bruyère L, Khoryati L, Bolland WH, Schwartz O, Lina B, Valette M, Thaunat O, Fassier JB; COVID-Ser study group; Pozzetto B, Paul S, Walzer T, Trouillet-Assant S. BA.1 breakthrough infection elicits distinct antibody and memory B cell responses in vaccinated-only versus hybrid immunity individuals. iScience. 2025 Feb 5;28(4):111962. doi: 10.1016/j.isci.2025.111962. PMID: 40224022; PMCID: PMC11987676.)_
Tsilioni I, Theoharides TC. Recombinant SARS-CoV-2 Spike Protein and Its Receptor Binding Domain Stimulate Release of Different Pro-Inflammatory Mediators via Activation of Distinct Receptors on Human Microglia Cells. Mol Neurobiol. 2023 Nov;60(11):6704-6714. doi: 10.1007/s12035-023-03493-7.
Rong Z, Mai H, Ebert G, Kapoor S, Puelles VG, Czogalla J, Hu S, Su J, Prtvar D, Singh I, Schädler J, Delbridge C, Steinke H, Frenzel H, Schmidt K, Braun C, Bruch G, Ruf V, Ali M, Sühs KW, Nemati M, Hopfner F, Ulukaya S, Jeridi D, Mistretta D, Caliskan ÖS, Wettengel JM, Cherif F, Kolabas ZI, Molbay M, Horvath I, Zhao S, Krahmer N, Yildirim AÖ, Ussar S, Herms J, Huber TB, Tahirovic S, Schwarzmaier SM, Plesnila N, Höglinger G, Ondruschka B, Bechmann I, Protzer U, Elsner M, Bhatia HS, Hellal F, Ertürk A. Persistence of spike protein at the skull-meninges-brain axis may contribute to the neurological sequelae of COVID-19. Cell Host Microbe. 2024 Dec 11;32(12):2112-2130.e10. doi: 10.1016/j.chom.2024.11.007. Epub 2024 Nov 29. PMID: 39615487.
Azer SA. COVID-19: pathophysiology, diagnosis, complications and investigational therapeutics. New Microbes New Infect. 2020 Sep;37:100738. doi: 10.1016/j.nmni.2020.100738.
Dingemans J, van der Veer BMJW, Gorgels KMF, Hackert V, den Heijer CDJ, Hoebe CJPA, Savelkoul PHM, van Alphen LB. Investigating SARS-CoV-2 breakthrough infections per variant and vaccine type. Front Microbiol. 2022 Nov 24;13:1027271. doi: 10.3389/fmicb.2022.1027271. PMID: 36504818; PMCID: PMC9729533.
Fontanet A, Autran B, Lina B, Kieny MP, Karim SSA, Sridhar D. SARS-CoV-2 variants and ending the COVID-19 pandemic. Lancet. 2021 Mar 13;397(10278):952-954. doi: 10.1016/S0140-6736(21)00370-6.
Andrews N, Stowe J, Kirsebom F, Toffa S, Sachdeva R, Gower C, Ramsay M, Lopez Bernal J. Effectiveness of COVID-19 booster vaccines against COVID-19-related symptoms, hospitalization and death in England. Nat Med. 2022 Apr;28(4):831-837. doi: 10.1038/s41591-022-01699-1. Epub 2022 Jan 14. PMID: 35045566; PMCID: PMC9018410.
Meeraus W, Stuurman AL, Durukal I, Conde-Sousa E, Lee A, Maria AS, Furtado BE, Ouwens M, Gray CM, Valverde DA, da Silva HG, Taylor S. COVID-19 vaccine booster doses provide increased protection against COVID-19 hospitalization compared with previously vaccinated individuals: Interim findings from the REFORCO-Brazil real-world effectiveness study during Delta and Omicron. Vaccine. 2023 Oct 6;41(42):6366-6378. doi: 10.1016/j.vaccine.2023.08.085. Epub 2023 Sep 12. PMID: 37704499.
Tarke A, Ramezani-Rad P, Alves Pereira Neto T, Lee Y, Silva-Moraes V, Goodwin B, Bloom N, Siddiqui L, Avalos L, Frazier A, Zhang Z, da Silva Antunes R, Dan J, Crotty S, Grifoni A, Sette A. SARS-CoV-2 breakthrough infections enhance T cell response magnitude, breadth, and epitope repertoire. Cell Rep Med. 2024 Jun 18;5(6):101583. doi:
Munoz FM, Cramer JP, Dekker CL, Dudley MZ, Graham BS, Gurwith M, Law B, Perlman S, Polack FP, Spergel JM, Van Braeckel E, Ward BJ, Didierlaurent AM, Lambert PH; Brighton Collaboration Vaccine-associated Enhanced Disease Working Group. Vaccine-associated enhanced disease: Case definition and guidelines for data collection, analysis, and presentation of im-munization safety data. Vaccine. 2021 May 21;39(22):3053-3066. doi: 10.1016/j.vaccine.2021.01.055. Epub 2021 Feb 23. PMID: 33637387; PMCID: PMC7901381.
Bigay J, Le Grand R, Martinon F, Maisonnasse P. Vaccine-associated enhanced disease in humans and animal models: Lessons and challenges for vaccine development. Front Microbiol. 2022 Aug 10;13:932408. doi: 10.3389/fmicb.2022.932408.
Ebenig A, Muraleedharan S, Kazmierski J, Todt D, Auste A, Anzaghe M, Gömer A, Postmus D, Gogesch P, Niles M, Plesker R, Miskey C, Gellhorn Serra M, Breithaupt A, Hörner C, Kruip C, Ehmann R, Ivics Z, Waibler Z, Pfaender S, Wyler E, Landthaler M, Kupke A, Nouailles G, Goffinet C, Brown RJP, Mühlebach MD. Vaccine-associated enhanced respiratory pathology in COVID-19 hamsters after TH2-biased immunization. Cell Rep. 2022 Aug 16;40(7):111214. doi: 10.1016/j.celrep.2022.111214. Epub 2022 Aug 3. PMID: 35952673; PMCID: PMC9346010.