Destacando brevemente algumas evidências não observadas em dois pacientes com COVID-19 e comorbidades
Conteúdo do artigo principal
Resumo
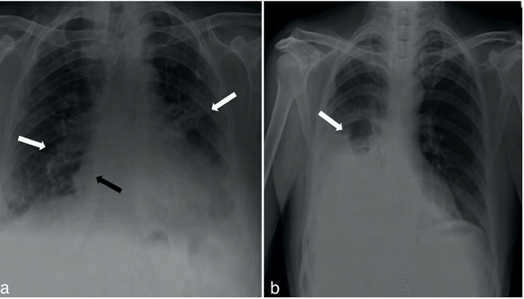
Nos últimos anos, o coronavírus da síndrome respiratória aguda grave 2 (SARS-CoV-2) causou significativa morbidade e mortalidade em todo o mundo. A positividade para COVID-19 dos pacientes foi confirmada por RT-PCR logo no início da hospitalização. Da mesma forma, os pacientes foram submetidos a radiografia de tórax, que revelou pneumonia por COVID-19 com derrame pleural no pulmão esquerdo. Todos os parâmetros laboratoriais, incluindo biomarcadores hematológicos (por exemplo, contagem total de leucócitos e hematócrito) e inflamatórios (por exemplo, proteína C-reativa, tempo de protrombina, tempo de tromboplastina parcial ativada, D-dímero e ferritina sérica) dos indivíduos falecidos estavam altamente anormais desde o primeiro dia. Choque séptico, neutrofilia, linfopenia, trombocitopenia e leucocitose foram evidentes em ambos os casos. Apesar de receberem tratamentos completos, as condições dos pacientes deterioraram rapidamente, retendo CO2 com baixa saturação de oxigênio. A pressão arterial e a saturação de oxigênio caíram acentuadamente, evoluindo para parada cardiorrespiratória nas fases finais em ambos os casos. Esses achados confirmam o impacto das comorbidades na gravidade da COVID-19, com base em mudanças notáveis nos parâmetros laboratoriais. O relatório atual sugere monitoramento extensivo de indivíduos com comorbidades e COVID-19 para reduzir a morbidade e mortalidade.
Detalhes do artigo

Este trabalho está licenciado sob uma licença Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
Referências
Marušić J, Hasković E, Mujezinović A, Dido V. Correlation of pre-existing comorbidities with disease severity in individuals infected with SARS-COV-2 virus. BMC Public Health. 2024 Apr 24:1053. doi: 10.1186/s12889-024-18457-2.
COVID-19 cases | WHO COVID-19 dashboard. Date accessed: 13/06/2024. Available from: https://data.who.int/dashboards/covid19/cases?n=c.
Chatterjee S, Nalla LV, Sharma M, Sharma N, Singh AA, Malim FM, Ghatage M, Mukarram M, Pawar A, Parihar N, Arya N, Khairnar, A. Association of COVID-19 with comorbidities: An update. ACS Pharmacol Transl Sci. 2023 Feb 6(3):334-354. doi: 10.1021/acsptsci.2c00181.
Hussain M, Samar Iltaf Sr, Salma Salman Sr, Ghuman F, Abbas S, Fatima M. Frequency of Comorbidities in Admitting COVID-19 Pneumonia patients in a tertiary care setup: An observational study. Cureus. 2021 Feb 25;13(2):e13546. doi: 10.7759/cureus.13546
Baral B, Saini V, Kandpal M, Kundu P, Dixit AK, Parmar HS, Menna AK, Trivedi P, Jha HC. The interplay of co-infections in shaping COVID-19 severity: expanding the scope beyond SARS-CoV-2. J Infect Public Health. 2024 Aug 17 (8) 102486. doi: 10.1016/j.jiph.2024.102486.
Russell CD, Lone NI, Baillie JK. Comorbidities, multimorbidity and COVID-19. Nat Med 2023 Feb 29:334–343. doi: 10.1038/s41591-022-02156-9.
Santos NCD, Miravitlles M, Camelier AA, Almeida VDC, Maciel RRBT, Camelier FWR. Prevalence and impact of comor-bidities in individuals with chronic obstructive pulmonary disease: A systematic review. Tuberc Respir Dis. 2022 Jul;85(3):205-220. doi: 10.4046/trd.2021.0179.
Morrow RL, Binka M, Li J, Irvine M, Bartlett SR, Wong S, Jeong D, Makuza JD, Wong J, Yu A, Krajden M, Janjua NZ. Impact of the COVID-19 pandemic on hepatitis C treatment initiation in British Columbia, Canada: An interrupted time series study. Viruses. 2024 Apr;16(5):655. doi: 10.3390/v16050655.
Afify S, Eysa B, Hamid FA, Abo-Elazm OM, Edris MA, Maher R, Abdelhalim A, Abdel Ghaffar MM, Omran DA, Shousha HI. Survival and outcomes for co-infection of chronic hepatitis C with and without cirrhosis and COVID-19: A multicenter ret-rospective study. World J Gastroenterol. 2021 Nov 11;27(42):7362-7375. doi: 10.3748/wjg.v27.i42.7362
Abdullah, Salman M, Muhammad R, Ali S, Attaullah, Khan M. Impact of laboratory biomarkers on COVID-19 severity: First cross-sectional study in a remote area of Pakistan. Glob J Med Pharm Biomed Update. 2024 Jun 10;19:6. doi: 10.25259/GJMPBU_79_2023.
Mirzaie H, Vahidi M, Shokoohi M, Darvishian M, Sharifi H, Sharafi H, Karamouzian M, Karamouzian. COVID-19 among patients with hepatitis B or hepatitis C: A systematic review. Hepat Mon. 2020 Dec 20(11); e111617. doi: 10.5812/hepatmon.111617.
Kulkarni A V., Kumar P, Tevethia HV, Premkumar M, Arab JP, Candia R, Talukdar R, Sharma M, Qi X, Rao PN, Reddy DN. Systematic review with meta-analysis: liver manifestations and outcomes in COVID-19. Aliment Pharmacol. 2020 Aug 1;52(4):584–99. doi: 10.1111/apt.15916.
Cerbu B, Pantea S, Bratosin F, Vidican I, Turaiche M, Frent S, Borsi E, Marincu I. Liver impairment and hematological changes in patients with chronic hepatitis C and COVID-19: A retrospective study after one year of pandemic. Medicina. 2021 Jun 10;57(6):597. doi: 10.3390/medicina57060597.
Xu XW, Wu XX, Jiang XG, Xu KJ, Ying LJ, Ma CL, Li SB, Wang HY, Zhang S, Gao HN, Sheng JF, Cai HL, Qiu YQ, Li LJ. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020 Feb 19;368. doi: 10.1136/bmj.m606.
Teimury A, Khameneh MT, Khaledi EM. Major coagulation disorders and parameters in COVID-19 patients. Eur J Med Res. 2022 Dec 1;27(1):1–10. doi: 10.1186/s40001-022-00655-6.
Niu J, Sareli C, Sareli A. 514. Clinical features and outcomes of 112 patients with SARS-CoV-2 infections requiring intensive care in a public healthcare system in South Florida. Open Forum Infect Dis. 2020 Dec 31;7(Suppl 1):S323. doi: 10.1093/ofid/ofaa439.708.
Zuwala-Jagiello J, Murawska-Cialowicz E, Pazgan-Simon M. Increased circulating advanced oxidation protein products and high-sensitive troponin T in cirrhotic patients with chronic hepatitis C: A preliminary report. Biomed Res Int. 2015 Jan 1;2015(1):786570. doi: 10.1155/2015/786570.
Iepsen UW, Plovsing RR, Tjelle K, Foss NB, Meyhoff CS, Ryrsø CK, Berg RMG, Secher NH. The role of lactate in sepsis and COVID-19: Perspective from contracting skeletal muscle metabolism. Exp Physiol. 2022 Jul 1;107(7):665–73. doi: 10.1113/EP089474.
Matsumori A, Shimada T, Chapman NM, Tracy SM, Mason JW. Myocarditis and heart failure associated with hepatitis C virus infection. J Card Fail. 2006 May 1;12(4):293–8. doi: 10.1016/j.cardfail.2005.11.004.
Pecly IMD, Azevedo RB, Muxfeldt ES, Botelho BG, Albuquerque GG, Diniz PHP, et al.. A review of Covid-19 and acute kidney injury: from pathophysiology to clinical results. Braz J Nephrol. 2021 Oct;43(4):551–571. doi: 10.1590/2175-8239-JBN-2020-0204.
Najera H, Ortega-Avila AG. Health and institutional risk factors of COVID-19 mortality in Mexico, 2020. Am J Prev Med. 2021 Apr 1;60(4):471–7. doi: 10.1016/j.amepre.2020.10.015.
Rahman MM, Hasan M, Ahmed A. potential detrimental role of soluble ACE2 in severe COVID-19 comorbid patients. Rev Med Virol. 2021 Sep 1;31(5):1–12. doi: 10.1002/rmv.2213.
Targher G, Mantovani A, Wang XB, Yan HD, Sun QF, Pan KH, Byrne CD, Zheng KI, Chen YP, Eslam M, George J, Zheng MH. Patients with diabetes are at higher risk for severe illness from COVID-19. Diabetes Metab. 2020 Sep 1;46(4):335. doi: 10.1016/j.diabet.2020.05.001.
Long H, Nie L, Xiang X, Li H, Zhang X, Fu X, Ren H, Liu W, Wang Q, Wu Q. D-Dimer and Prothrombin time are the significant indicators of severe COVID-19 and poor prognosis. Biomed Res Int. 2020 Jan 1;2020(1):6159720. doi: 10.1155/2020/6159720.
Tugba Bozkurt F, Tercan M, Patmano G, Bingol Tanrıverdi T, Avni Demir H, Fahri Yurekli U. Can ferritin levels predict the severity of illness in patients with COVID-19? 2021;13(1) doi: 10.7759/cureus.12832.
Hertanto DM, Sutanto H, Adi S. Case Report: Diabetic nephropathy aggravates the progression and prognosis of COVID-19-associated acute limb ischemia. F1000Res. 2021;10. doi: 10.12688/f1000research.54193.2.
Mirjalili H, Dastgheib SA, Shaker SH, Bahrami R, Mazaheri M, Sadr-Bafghi SMH, Sadeghizadeh-Yazdi J, Neamatzadeh H. Proportion and mortality of Iranian diabetes mellitus, chronic kidney disease, hypertension and cardiovascular disease pa-tients with COVID-19: a meta-analysis. J Diabetes Metab Disord. 2021 Jun 1;20(1):905–17. doi: 10.1007/s40200-021-00768-5.