Unilateral Thyroid Involvement in Graves' Disease: A rare presentation of Graves’ Disease
Main Article Content
Abstract
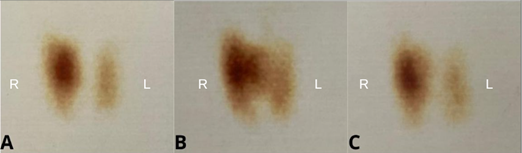
Graves' disease is a rare autoimmune disorder characterized by increased hormone production leading to clinical signs of hyperthyroidism, most cases present with different degrees of TSH suppression, accompanied by elevated FT4. Thyroid scintigraphy commonly reveals an enlarged goiter with diffuse increased iodine uptake. This study presents the case of a 50-year-old woman with a clinical history of Graves' disease presenting with suppressed TSH and elevated FT4 combined with clinical signs of hyperthyroidism (tachycardia and peripheral tremors). Thyroid imaging showed increased unilateral uptake on scintigraphy with no visible nodules on ultrasound. The patient showed an adequate initial response to methimazole, with disease relapses after dose reduction. The patient was able to maintain euthyroidism with continued antithyroid drug use. Single lobe involvement of Graves' Disease is a rare phenomenon attributed to the autoimmune process combined with acquired variations impacting a specific lobe. Clinically, patients are present with different degrees of hyperthyroidism. In most cases, the use of antithyroid drugs provides adequate disease control, with patients subjected to definitive treatment presenting a higher risk of disease recurrence in the contralateral lobe. This report shows a case with a favorable response to continue antithyroid drugs treatment after disease relapse. The findings highlight the rare occurrence of unilateral thyroid gland involvement in Graves' disease. Also, suggest a favorable response to continue antithyroid treatment for patients exhibiting relapses.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Lanzolla G, Marinò M, Menconi F. Graves disease: latest understanding of pathogenesis and treatment options. Nat Rev Endocrinol. 2024;20(11):647–660. doi:10.1038/s41574-024-01016-5.
Hussain YS, Hookham JC, Allahabadia A, Balasubramanian SP. Epidemiology, management and outcomes of Graves’ dis-ease—real life data. Endocrine. 2017;56(3):568–578. doi:10.1007/s12020-017-1306-5.
Diana T, Olivo PD, Kahaly GJ. Thyrotropin receptor blocking antibodies. Horm Metab Res. 2018;50(12):853–862. doi:10.1055/a-0723-9023.
Burch HB. Overview of the clinical manifestations of thyrotoxicosis. In: Braverman LE, editor. Diseases of the Thyroid. Vol. 10. Baltimore: Williams & Wilkins; 2013.
Smith TJ, Hegedüs L. Graves’ disease. N Engl J Med. 2016;375(16):1552–1565. doi:10.1056/NEJMra1510030.
Scappaticcio L, Trimboli P, Keller F, Imperiali M, Piccardo A, Giovanella L. Diagnostic testing for Graves’ or non-Graves’ hyperthyroidism: a comparison of two thyrotropin receptor antibody immunoassays with thyroid scintigraphy and ultra-sonography. Clin Endocrinol (Oxf). 2020;92(2):169–178. doi:10.1111/cen.14130.
Dimai HP, Ramschak-Schwarzer S, Lax S, Lipp RW, Leb G. Hyperthyroidism of Graves’ disease: evidence for only unilateral involvement of the thyroid gland in a 31-year-old female patient. J Endocrinol Invest. 1999;22(3):215–219. doi:10.1007/BF03343545.
Kalawat T, Manthri R, Ajit N, Vaikakkara S, Devi B. Unilateral Graves’ disease: the lesser known. Indian J Nucl Med. 2019;34(2):96. doi:10.4103/ijnm.ijnm_11_19.
Wagih S. Graves’ disease affecting one thyroid lobe (unilateral Graves’ disease): case report. Egypt J Nucl Med. 2010;3(3):62–65. doi:10.21608/egyjnm.2010.5501.
Sakata S, Fuwa Y, Goto S, Fukui M, Yuasa H, Takuno H, et al. Two cases of Graves’ disease with presentation of unilateral diffuse uptake of radioisotopes. J Endocrinol Invest. 1993;16(11):903–907. doi:10.1007/BF03348954.
Gratz S, Barth P, Arnold R, Behr TM. Graves’ disease with unilateral radioisotope uptake. Nuklearmedizin. 2004;43(5):N66–N68.
Bolognesi M, Rossi R. Case history: unilateral Graves’ disease. Thyroid. 2006;16(5):493–495. doi:10.1089/thy.2006.16.493.
Chen LC, Green JB. First reported case of unilateral Graves’ disease in the left lobe of a bilobar thyroid gland. Thyroid. 2011;21(6):683–686. doi:10.1089/thy.2010.0343.
Alzedaneen Y, Moxley MC, Reddy R, Munir KM. Unilateral thyroid lobe involvement of Graves disease. JCEM Case Rep. 2023;1(2):luad023. doi:10.1210/jcemcr/luad023.
Bu Bshait MS. Graves’ disease with only unilateral involvement: a case report. Int J Surg Case Rep. 2024;114:109138. doi:10.1016/j.ijscr.2023.109138.
Elamari S, Rhmari Tlemcani FZ, Motaib I, Laidi S, Chadli A. Graves’ disease affecting one thyroid lobe: about 2 cases. Med Nucl (Paris). 2022;46(3):164–167. doi:10.1016/j.mednuc.2022.03.001.
Antonelli A, Ferrari SM, Ragusa F, Elia G, Paparo SR, Ruffilli I, et al. Graves’ disease: epidemiology, genetic and environmental risk factors and viruses. Best Pract Res Clin Endocrinol Metab. 2020;34(1):101387. doi:10.1016/j.beem.2020.101387.
Cooper DS. Antithyroid drugs for the treatment of hyperthyroidism caused by Graves’ disease. Endocrinol Metab Clin North Am. 1998;27(1):225–247. doi:10.1016/S0889-8529(05)70308-X.
Villagelin D, Cooper DS, Burch HB. A 2023 international survey of clinical practice patterns in the management of Graves disease: a decade of change. J Clin Endocrinol Metab. 2024;109(11):2956–2966. doi:10.1210/clinem/dgae222.
Villagelin D, Romaldini JH, Santos RB, Milkos AB, Ward LS. Outcomes in relapsed Graves’ disease patients following radi-oiodine or prolonged low dose of methimazole treatment. Thyroid. 2015;25(12):1282–1290. doi:10.1089/thy.2015.0195.
Volpé R. The immunomodulatory effects of anti-thyroid drugs are mediated via actions on thyroid cells, affecting thyrocyte–immunocyte signalling: a review. Curr Pharm Des. 2001;7(6):451–460. doi:10.2174/1381612013397898.