Role of nutritional therapy in the post-COVID syndrome rehabilitation process: a case report
Main Article Content
Abstract
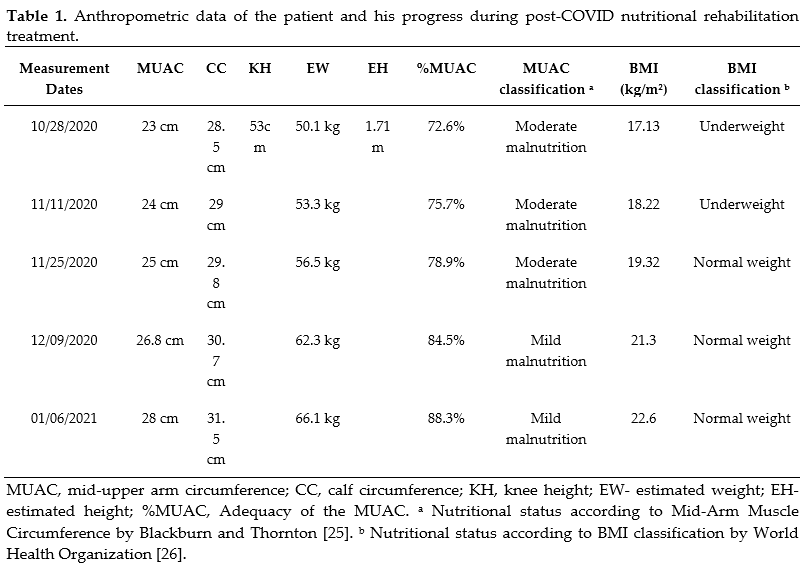
The COVID-19 pandemic originated in Wuhan, China, and quickly became a global concern. Risk factors for complications, apart from age, are closely related to nutrition. In hospitalized patients, extended stays can lead to malnutrition and sarcopenia, highlighting nutrition's pivotal role in managing and alleviating symptoms. This study explores the efficacy of nutritional therapy for post-COVID patients within the Home Care Program framework. Following hospital discharge, the patient was enrolled in the Home Care Program and showed symptoms such as post-COVID-19 condition, significant pressure injury, low weight, and muscular atrophy. A multi-professional developed a therapeutic plan with a focus on nutrition. Within 70 days, a 58-year-old male patient, supported by nutritional supplementation including arginine, proline, and vital vitamins and minerals, exhibited considerable health improvements. These included a progression of nutritional status to eutrophy, a weight gain of 6 kg since the beginning of the intervention, and a 15.7% increase in MUAC adequacy. The nutritional intervention also effectively tackled issues like constipation. These enhancements enabled the patient to respond better to physical therapy, reclaiming significant daily activity autonomy. Comprehensive nutritional therapy is instrumental for recovering post-COVID-19 patients, accentuating the importance of personalized care in ensuring patient well-being and autonomy.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
1. Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91(1):157-160. doi:10.23750/abm.v91i1.9397
Weston S, Frieman MB. COVID-19: knowns, unknowns, and questions. Msphere. 2020;5(2):1-5.
Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi:10.1016/j.jaut.2020.102433
Xie P, Ma W, Tang H, Liu D. Severe COVID-19: a review of recent progress with a look toward the future. Front Public Health. 2020;8:1-7. doi:10.3389/fpubh.2020.00189
Yuki K, Fujiogi M, Koutsogiannaki S. COVID-19 pathophysiology: A review. Clin Immunol. 2020;1-7. doi:10.1016/j.clim.2020.108427
Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL et al. Practical recommendations for the man-agement of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 2020;8(6):546-550. doi:10.1016/S2213-8587(20)30152-2
Muscogiuri G, Pugliese G, Barrea L, Savastano S, Colao A. Commentary: Obesity: The “Achilles heel” for COVID-19?. Me-tabolism. 2020;108:154251. doi:10.1016/j.metabol.2020.154251
Zhang P, He Z, Yu G, Peng D, Feng Y, Ling J et al. The modified NUTRIC score can be used for nutritional risk assessment as well as prognosis prediction in critically ill COVID-19 patients. Clin Nutr. 2021;40(2):534-541. doi:10.1016/j.clnu.2020.05.051
Petrilli CM, Jones SA, Yang J, Rajagopalan H, O’Donnel L, Chernyak Y et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;1-15. doi:10.1136/bmj.m1966
Danziato-Neto MA, Barbosa CL, Melo ANMV, Câmara CRS, Carioca AAF, Silva CAB, et al. Obesity decreases energy and protein intake in hospitalized COVID-19 patients undergoing continuous positive airway pressure treatment. Nutr Res. 2023;118:52–62. doi:10.1016/j.nutres.2023.07.006
Anker MS, Landmesser U, Haehling S, Butler J, Coats AJS, Anker SD. Weight loss, malnutrition, and cachexia in COVID-19: facts and numbers. J Cachexia Sarcopenia Muscle. 2020;12(1):9–13. doi:10.1002/jcsm.12674
Iqbal FM, Lam K, Sounderajah V, Clarke JM, Ashrafian H, Ara Darzi. Characteristics and predictors of acute and chronic post-COVID syndrome: a systematic review and meta-analysis. EClinicalMedicine. 2021;36. doi:10.1016/j.eclinm.2021.100899
NICE guideline. COVID-19 rapid guideline: managing the long-term effects of COVID-19. NICE; 2020. https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/
Barrea L, Grant WB, Frias-Toral E, Vetrani C, Verde L, De Alteriis G, et al. Dietary Recommendations for Post-COVID-19 Syndrome. Nutrients. 2022;14(6):1305. doi:10.3390/nu14061305
Crispo A, Bimonte S, Porciello G, Forte CA, Cuomo G, Montagnese C et al. Strategies to evaluate outcomes in long-COVID-19 and post-COVID survivors. Infect Agent Cancer. 2021;16(1):1-20. doi:10.1186/s13027-021-00401-3
Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Cuidados em terapia nutricional. 1. ed., 1. reimpr. Brasília: Ministério da Saúde; 2015.
Campos LF, Barreto PA, Ceniccola GD, Gonçalves RC, Matos LBN, Zambelli CMSF et al. Revisão do parecer BRASPEN de terapia nutricional em pacientes hospitalizados com COVID-19. Braspen J. 2021;36:1-4. doi:10.37111/braspenj.COVID2021
World Health Organization (WHO). Coronavirus disease (COVID-19) weekly epidemiological update and weekly opera-tional update. 2021. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
Zhou T, Yang K, Thapa S, Liu H, Wang B, Yu S, et al. Differences in symptom burden among cancer patients with different stages of cachexia. J Pain Symptom Manage. 2017;53(5):919–926. doi:10.1016/j.jpainsymman.2016.12.325
Vaes RDW, Welbers TTJ, Van Dijk DPJ, Rennspiess D, Hausen AZ, Damink SWMO, et al. Intestinal smooth muscle aberrations in pancreatic cancer patients with sarcopenia. JCSM Rapid Commun. 2021;4(2):187–196. doi:10.1002/rco2.34
Albaugh VL, Mukherjee K, Barbul A. Proline precursors and collagen synthesis: biochemical challenges of nutrient sup-plementation and wound healing. J Nutr. 2017;147(11):2011-7. doi:10.3945/jn.117.256404
Berger MM, Shenkin A, Schweinlin A, Amrein K, Augsburger M, Biesalski H-K et al. ESPEN micronutrient guideline. Clin Nutr. 2022;41(6):1357–424. doi:10.1016/j.clnu.2022.02.015
Bharucha AE, Sharma M. Painful and Painless Constipation: All Roads Lead to (a Change in) Rome. Dig Dis Sci. 2018;63(7):1671–4. doi:10.1007/s10620-018-5027-2
Everhart JE, Go VL, Johannes RS, Fitzsimmons SC, Roth HP, White LR. A longitudinal survey of self-reported bowel habits in the United States. Dig Dis Sci. 1989;34(8):1153–62. doi:10.1007/BF01537261
Blackburn GL, Thornton PA. Nutritional assessment of the hospitalized patient. Med Clin North Am. 1979;63:11103-15.
World Health Organization. A healthy lifestyle - WHO recommendations [Internet]. Geneva: World Health Organization; 2010. [cited 2023 Jul 17]. Available from: https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations.