Remember Leptospirosis: two cases report
Conteúdo do artigo principal
Resumo
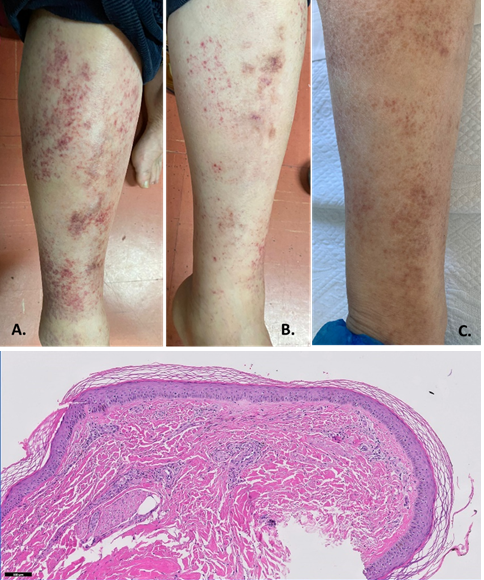
Leptospirosis has a wide variety of clinical manifestations, from asymptomatic to vital organ involvement. Its significant morbidity highlights the importance of recognizing and identifying how leptospirosis can be acquired and transmitted. With adequate management, the disease can be treated with no complications. The authors describe two patients, a couple from a rural area in Portugal, presenting with different manifestations of the same disease a month apart between hospitalizations. Both experienced kidney and liver dysfunction, and although having different therapeutic approaches, both had a favorable evolution. Recognition of leptospirosis based on clinical symptoms and specific laboratory clues may allow early initiation of therapy. Occupational exposure is a significant risk factor. Vaccination and awareness programs are essential for reducing the risk.
Detalhes do artigo

Este trabalho está licenciado sob uma licença Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
Referências
Wawrzynowicz-Syczewska M (2022) Leptospirosis. McMaster Textbook of Internal Medicine. Kraków: Medycyna Praktyczna.
Warnasekara J, Srimantha S, Kappagoda C, Jayasundara D, Senevirathna I, et al. (2022) Diagnostic method-based underes-timation of leptospirosis in clinical and research settings; an experience from a large prospective study in a high endemic setting. PLOS Neglected Tropical Diseases. 16(4): e0010331.
Haake DA, Levett PN (2015) Leptospirosis in humans. Curr Top Microbiol Immunol. 387: 65-97.
Vieira ML, Gama-Simões MJ, Collares-Pereira M (2006) Human leptospirosis in Portugal: a retrospective study of eighteen years. International Journal of Infectious Diseases. 10(5): 378-86.
De Brito T, Silva AMGD, Abreu PAE (2018) Pathology and pathogenesis of human leptospirosis: a commented review. Rev. Inst. Med. trop. S. Paulo. 60: e23.
Levett PN (2001) Leptospirosis. Clin Microbiol Rev. 14(2): 296-326.
Seguro AC, Lomar AV, Rocha AS (1990) Acute renal failure of leptospirosis: Nonoliguric and hypokalemic forms. Nephron .55(2): 146-151.
Lee B, Rose E (2018) Other Potentially Life-Threatening Conditions with Mucocutaneous Findings (Leptospirosis, Typhoid Fever, Dengue, Diphtheria, Murine Typhus). Life-Threatening Rashes. 12: 319–347.
Charan J, Saxena D, Mulla S, Yadav P (2013) Antibiotics for the treatment of leptospirosis: systematic review and meta-analysis of controlled trials. Int J Prev Med. 4(5):501–510.
Raptis L, Pappas G, Akritidis N (2006) Use of ceftriaxone in patients with severe leptospirosis. Int J Antimicrob Agents. 28(3): 259–61.
Brett-Major DM, Coldren R (2012) Antibiotics for leptospirosis. Cochrane Database of Systematic Reviews. 15(2): CD008264.
Rivero SM, Rago M (2011) Leptospirosis: revisión del tema a propósito de dos casos. Biomedicina. 6(2): 38-49.
Centers for Disease Control and Prevention (2015) Leptospirosis – Prevention. Available in http://www.cdc.gov/leptospirosis/pets/prevention/index.html.